Published online Jul 16, 2015. doi: 10.12998/wjcc.v3.i7.650
Peer-review started: January 28, 2015
First decision: March 20, 2015
Revised: April 13, 2015
Accepted: May 16, 2015
Article in press: May 18, 2015
Published online: July 16, 2015
Processing time: 182 Days and 12.3 Hours
Perifollicular granuloma is a unique histologic feature and whether it is associated with immunoglobulin G4 (IgG4)-related disease is controversial. We report a case of a 38-year-old man who presented with worsening left eye pain, proptosis, tearing, gritty sensation, blurred vision and multiple lymphadenopathy. An axillary lymph node resection showed reactive follicular and interfollicular lymph node hyperplasia, and increased eosinophils and plasma cells (at least 80% of IgG+ plasma cells were positive for IgG4). A distinct feature was the presence of multifocal, perifollicular histiocytic granulomas, which formed a wreath around the entire follicles. The human herpes virus 8 was not detected by immunohistochemistry. In addition, an extensive panel of special stains, immunohistochemistry, and flow cytometry was negative for lymphoma, fungal, or mycobacterial infection. The findings were suggestive of IgG4-related sclerosing disease-associated lymphadenopathy. Further laboratory testing showed a significant increase of serum immunoglobulin E (> 23000 IU/mL) and slight increase of total IgG, but normal serum IgG4. Even though perifollicular granuloma is a nonspecific histopathologic feature and can be seen in other diseases, such as nodular lymphocyte predominant Hodgkin lymphoma, IgG4-related lymphadenopathy should be listed in the differential diagnoses of benign reactive lymph nodes, especially when perifollicular granuloma and plasmacytosis coexist.
Core tip: We report a case of a 38-year-old man who presented with worsening left eye pain and multiple lymphadenopathy. An axillary lymph node resection showed increased eosinophils and plasma cells (at least 80% of immunoglobulin (Ig)G+ plasma cells were positive for IgG4 and the presence of multifocal, perifollicular histiocytic granulomas, which formed a wreath around the entire follicles. An extensive workup was negative for lymphoma, fungal, or mycobacterial infection. The findings were suggestive of IgG4-related sclerosing disease-associated lymphadenopathy. Thus, IgG4-related lymphadenopathy should be listed in the differential diagnoses of benign reactive lymph nodes, especially when perifollicular granuloma and plasmacytosis coexist.
- Citation: Liang L, Zhou J, Chen L. Perifollicular granulomas with IgG4 plasmacytosis: A case report and review of literature. World J Clin Cases 2015; 3(7): 650-654
- URL: https://www.wjgnet.com/2307-8960/full/v3/i7/650.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i7.650
Immunoglobulin G4 (IgG4)-related disease is a recently recognized fibro-inflammatory condition that can involve multiple organs and cause tumor-like enlargement[1,2]. It is characterized by a lymphoplasmacytic infiltrate enriched in IgG4-positive plasma cells, while elevated serum concentrations of IgG4 are found in 60% to 70% of patients[3]. IgG4-related disease has a male predilection (male to female ratio 8:1)[4].
According to the consensus statement from a multinational, multidisciplinary group of experts, the major histopathological features to make the diagnosis of IgG4-related disease include a dense lymphoplasmacytic infiltrate, plasma cells, storiform fibrosis, and obliterative phlebitis[5]. However, these features are usually uncommonly seen in certain organs, such as lymph nodes.
We describe a case of a 38-year-old man with swelling of soft tissue surround the eye and multiple lymphadenopathy and an axillary lymph node resection showed reactive follicular and interfollicular lymph node hyperplasia, increased eosinophils and plasma cells (at least 80% of immunoglobulin IgG+ plasma cells were positive for IgG4) and multifocal, perifollicular histiocytic granulomas, which formed a wreath around the entire follicles. Review of literature also found our findings may add to the knowledge of IgG4-related disease.
We report a case of a 38-year-old man who presented with worsening left eye pain, proptosis, tearing, gritty sensation, and blurred vision. Magnetic resonance imaging of orbits confirmed enlargement of the left medial rectus, superior oblique and inferior rectus muscle, and enhancing soft tissue signal encasing the left optic nerve sheath. Computed tomography scan of chest and abdomen showed multiple lymphadenopathy. Clinically, lymphoma was suspected. Patient’s rheumatology work up was negative, including anti-neutrophil cytoplasmic antibodies, anti-double stranded DNA, anti-nuclear antibodies, anti-Smith, anti-ribonucleoprotein, anti-complement C3 and C4. Complete blood count shown mild eosinophilia, otherwise, it was unremarkable.
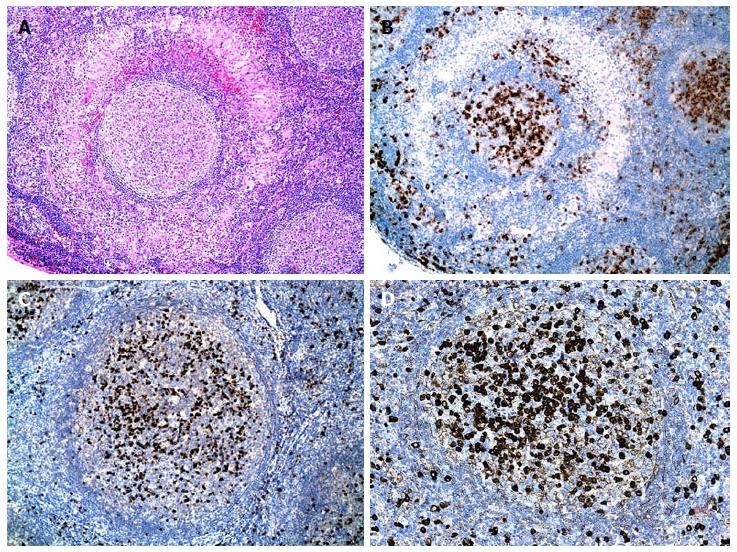
An axillary lymph node resection showed reactive follicular and interfollicular lymph node hyperplasia, and increased eosinophils and plasma cells (at least 80% of IgG+ plasma cells were positive for IgG4). A distinct feature was the presence of multifocal, perifollicular histiocytic granulomas, which formed a wreath around the entire follicles (Figure 1A). Increased plasma cells were marked by CD138 immunohistochemical stain (Figure 1B). IgG4+ plasma cells are markedly increased (Figure 1D), compared with total IgG stain (Figure 1C). EBER (EBV encoded small RNA by in situ hybridization) was negative. The human herpes virus 8 was not detected by immunohistochemistry. In addition, an extensive panel of special stains, immunohistochemistry, and flow cytometry was negative for lymphoma, fungal, or mycobacterial infection. The findings were suggestive of IgG4-related sclerosing disease-associated lymphadenopathy.
Further laboratory testing showed a significant increase of serum IgE (> 23000 IU/mL) and slight increase of total IgG (1802 mg/dL), but normal serum IgG4 (27 mg/dL). The patient was started on prednisone and methotrexate with reduction in proptosis and in the size of orbital mass by computerized tomography (CT) scan. While patient was maintained with methotrexate and tapering on steroid, he was noted to have left eye redness and itching. Rituximab was added and methotrexate was discontinued. The patient’s symptom subsided.
According to the consensus statement from a multinational, multidisciplinary group of experts, the major histopathological features to make the diagnosis of IgG4-related disease include a dense lymphoplasmacytic infiltrate, plasma cells, storiform fibrosis, and obliterative phlebitis[5]. However, these features are usually not seen in certain organs, such as lymph nodes. Fibrosis and obliterative phlebitis are usually not present in lymph nodes.
Lymph nodes in IgG4-related disease may show variable histopathologic features. Cheuk et al[4] divided it into five different categories, including multicentric Castleman disease-like (type I), follicular hyperplasia (type II), interfollicular expansion (type III), progressive transformation of germinal centers (type IV), and inflammatory pseudotumor-like (type V). Nevertheless, an increase in IgG4+ plasma cells with an IgG4/IgG plasma cell ratio exceeding 0.4, and/or an absolute number of IgG4+ plasma cells of more than 50/high-power field (hpf) are the currently accepted cutoff for IgG4-related disease. However, presence of IgG4+ plasma cells in isolated reactive lymphadenopathy is not exclusively specific for IgG4-related disease[6]. Martinez et al[6] reported seven of the 55 solitary reactive lymph nodes with increased IgG4/IgG plasma cell ratio of more than 0.4, and six of them showed more than 50 IgG4+ plasma cells per high power field, but none of these patients had history of IgG4-related disease. On the other hand, Uehara et al[7] reported that presence of fibrosis in lymph nodes, together with increased IgG4 ratio and other features of IgG4-related disease, may suggest the diagnosis of IgG4-related lymphadenopathy.
Even though epithelioid cell granulomas is usually not considered a feature of IgG4-related disease at extranodal sites, it has been described in lymph nodes. Siddiqi et al[8] described seven cases with perifollicular granuloma in a concentric or crescent-like arrangement encircling lymphoid follicles and associated with a marked elevation of intra-germinal center IgG4+ plasma cells. However, the specificity of these findings were debated by Cheuk et al[4]. Grimm et al[9] reported histiocytic proliferation in 11 of 29 cases of lymphadenopathy with increased IgG4 plasma cells, and a prominent ringing of follicules by epithelioid histiocytes in 3 patients (Table 1). In addition, Takahashi et al[10] reported a case of IgG4-related lymphadenopathy with prominent granulomatous inflammation, most likely due to reactivation of Epstein-Barr virus. Takeuchi et al[11] performed Epstein-Barr virus (EBV)-encoded RNA (EBER) in situ hybridization and identified EBER-positive cells in 18 of 31 cases (58%) of IgG4-related lymphadenopathy, significantly higher rate than non-IgG4-related reactive lymphoid hyperplasia. However, EBER was negative in our case, and either negative or rarely positive in the two cases with EBER performed in Grimm group’s study (Table 1). Further study is needed to determine whether there is a causal relationship.
| Case | Ref. | Age (yr) | Gender | Location | IgG4/IgG ratio | Eosinophils | Fibrosis | EBER |
| 1 | Siddiqi et al[8] | 47 | M | Cervical | 0.7 | Mild | Marked | NA |
| 2 | Siddiqi et al[8] | 63 | M | Axillary | 0.7 | None | None | NA |
| 3 | Siddiqi et al[8] | 50 | F | Cervical | 0.5 | Minimal | Mild | NA |
| 4 | Siddiqi et al[8] | 34 | M | Cervical | 0.6 | None | None | NA |
| 5 | Siddiqi et al[8] | 12 | M | Cervical | 0.7 | Mild | None | NA |
| 6 | Siddiqi et al[8] | 58 | M | Unknown | 0.7 | None | None | NA |
| 7 | Siddiqi et al[8] | 83 | M | Axillary | 0.7 | Mild | Mild | NA |
| 8 | Grimm et al[9] | 47 | M | Cervical | > 0.4 | NA | NA | NA |
| 9 | Grimm et al[9] | 58 | F | NA | > 0.4 | NA | NA | Negative |
| 10 | Grimm et al[9] | 83 | M | Axillary | > 0.4 | NA | Present | Rarely positive |
| 11 | Current case | 38 | M | Axillary | > 0.8 | Increased | None | NA |
IgG4-related disease is a great mimicker. One of the differential diagnoses is multicentric Castleman’s disease. However, IgG4+/IgG+ plasma cell ratio is usually less than 0.4 in multicentric Castleman disease. Furthermore, elevated serum levels of interleukin-6 and vascular endothelial growth factor favor the diagnosis of multicentric Castleman’s disease[12]. Rosai-Dorfman disease can also show increased IgG4-positive plasma cells, as well as other autoimmune diseases including rheumatoid lymphadenopathy, are also in the differential diagnosis[13,14]. Moreover, bacterial, viral, fungal and parasitic infections have to be carefully ruled out. In our case, special stains and cultures were performed and the results were negative. The patient recovered quickly after immunosuppressive therapy, which was not consistent with infectious lymphadenitis. Other diseases with perifollicular granuloma have been reported, including reactive lymph nodes of unknown etiology, progressive transformation of germinal centers, and nodular lymphocyte predominance Hodgkin lymphoma[4]. However, in our case, morphologic features, immunohistochemistry and flow cytometry results were not consistent with lymphoma.
In our case, the pathologic evaluation is based on lymph node resection specimen. Even though biopsy of the orbital lesion was considered in initial evaluation, it wasn’t performed based on the decision of multidisciplinary team, because this invasive procedures carried a significant risk. In addition, our patient had a normal serum level of IgG4. It is a not uncommon finding and is seen in up to 40% of patients with IgG4-related disease[3]. Our patient was treated with prednisone, methotrexate and Rituximab. His eye symptoms subsided dramatically and a post-treatment imaging study showed shrinking of the orbital mass. Thus, clinical presentations and histopathologic findings in this case supported of a diagnosis of IgG4-related disease.
According to the most recently published International consensus guidance statement, the first line treatment of active IgG4-related disease are glucocorticoids, but a combination of glucocorticoids and a steroid-sparing immunosuppressive agent (e.g., azathioprine, methotrexate or mycophenolate) may be beneficial for some patients[15]. In addition, Rituximab has been reported to be an effective drug to treat patients with IgG4-related ophthalmopathy, especially those intolerant of steroid or with recurrent or refractory disease[16].
In summary, we described a case of IgG4-related disease with distinct features of perifollicular granulomas and literature reviews. This may expand our knowledge of pathologic findings of IgG4-related disease in a lymph node, although clinical history, lab results and radiological findings must be taken into consideration when making the diagnosis.
A 38-year-old man who presented with worsening left eye pain, proptosis, tearing, gritty sensation and blurred vision.
Multiple lymphadenopathy was identified.
Lymphoma, Castleman’s disease, fungal or mycobacterial infection, autoimmune disorders, etc.
Serum immunoglobulin E (> 23000 IU/mL) and slight increase of total immunoglobulin G (IgG), but normal serum IgG4. An extensive panel of special stains, immunohistochemistry, and flow cytometry was negative for lymphoma, fungal, or mycobacterial infection.
Magnetic resonance imaging of orbits showed enlargement of the left medial rectus, superior oblique and inferior rectus muscle, and enhancing soft tissue signal encasing the left optic nerve sheath. Computed tomography scan of chest and abdomen showed multiple lymphadenopathy.
An axillary lymph node resection showed reactive follicular and interfollicular lymph node hyperplasia, and increased eosinophils and plasma cells (at least 80% of IgG+ plasma cells were positive for IgG4). A distinct feature was the presence of multifocal, perifollicular histiocytic granulomas, which formed a wreath around the entire follicles.
The patient was started on prednisone and methotrexate with reduction in proptosis and in the size of orbital mass by computerized tomography scan. While patient was maintained with methotrexate and tapering on steroid, he was noted to have left eye redness and itching. Rituximab was added and methotrexate was discontinued. The patient’s symptom subsided.
Perifollicular granuloma is a unique histologic feature and whether it is associated with IgG4-related disease is controversial. Very few cases have been reported in the English literature.
IgG4-related disease is a recently recognized fibro-inflammatory condition that can involve multiple organs and cause tumor-like enlargement, which is characterized by a lymphoplasmacytic infiltrate enriched in IgG4-positive plasma cells.
IgG4-related lymphadenopathy should be listed in the differential diagnoses of benign reactive lymph nodes, especially when perifollicular granuloma and plasmacytosis coexist.
The authors have performed a good study, the manuscript is interesting.
P- Reviewer: Gonzalez-Granado LI, Sugimura H S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
| 1. | Zen Y, Nakanuma Y. IgG4-related disease: a cross-sectional study of 114 cases. Am J Surg Pathol. 2010;34:1812-1819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 419] [Cited by in RCA: 402] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 2. | Palazzo E, Palazzo C, Palazzo M. IgG4-related disease. Joint Bone Spine. 2014;81:27-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Sah RP, Chari ST. Serologic issues in IgG4-related systemic disease and autoimmune pancreatitis. Curr Opin Rheumatol. 2011;23:108-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 242] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 4. | Cheuk W, Chan JK. Lymphadenopathy of IgG4-related disease: an underdiagnosed and overdiagnosed entity. Semin Diagn Pathol. 2012;29:226-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 101] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | Deshpande V, Zen Y, Chan JK, Yi EE, Sato Y, Yoshino T, Klöppel G, Heathcote JG, Khosroshahi A, Ferry JA. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25:1181-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1714] [Cited by in RCA: 1757] [Article Influence: 135.2] [Reference Citation Analysis (0)] |
| 6. | Martinez LL, Friedländer E, van der Laak JA, Hebeda KM. Abundance of IgG4+ plasma cells in isolated reactive lymphadenopathy is no indication of IgG4-related disease. Am J Clin Pathol. 2014;142:459-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Uehara T, Masumoto J, Yoshizawa A, Kobayashi Y, Hamano H, Kawa S, Oki K, Oikawa N, Honda T, Ota H. IgG4-related disease-like fibrosis as an indicator of IgG4-related lymphadenopathy. Ann Diagn Pathol. 2013;17:416-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Siddiqi IN, Brynes RK, Grimm K, O’Malley DP, Wang E. Perifollicular granulomatous inflammation in reactive lymph nodes: a possible morphologic marker for IgG4 plasmacytosis. J Hematopathol. 2011;4:207–214. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Grimm KE, Barry TS, Chizhevsky V, Hii A, Weiss LM, Siddiqi IN, Brynes RK, O’Malley DP. Histopathological findings in 29 lymph node biopsies with increased IgG4 plasma cells. Mod Pathol. 2012;25:480-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Takahashi E, Kojima M, Kobayashi M, Kitamura A, Yokoi T, Hara K, Nakamura S. Primary IgG4-related lymphadenopathy with prominent granulomatous inflammation and reactivation of Epstein-Barr virus. Virchows Arch. 2012;460:225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Takeuchi M, Sato Y, Yasui H, Ozawa H, Ohno K, Takata K, Gion Y, Orita Y, Tachibana T, Itoh T. Epstein-Barr virus-infected cells in IgG4-related lymphadenopathy with comparison with extranodal IgG4-related disease. Am J Surg Pathol. 2014;38:946-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Izumi Y, Takeshita H, Moriwaki Y, Hisatomi K, Matsuda M, Yamashita N, Kawahara C, Shigemitsu Y, Iwanaga N, Kawakami A. Multicentric Castleman disease mimicking IgG4-related disease: A case report. Mod Rheumatol. 2014;1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Zhang X, Hyjek E, Vardiman J. A subset of Rosai-Dorfman disease exhibits features of IgG4-related disease. Am J Clin Pathol. 2013;139:622-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Asano N, Sato Y. Rheumatoid lymphadenopathy with abundant IgG4(+) plasma cells : a case mimicking IgG4-related disease. J Clin Exp Hematop. 2012;52:57-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Khosroshahi A, Wallace ZS, Crowe JL, Akamizu T, Azumi A, Carruthers MN, Chari ST, Della-Torre E, Frulloni L, Goto H. International Consensus Guidance Statement on the Management and Treatment of IgG4-Related Disease. Arthritis Rheumatol. 2015;67:1688-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 573] [Cited by in RCA: 665] [Article Influence: 66.5] [Reference Citation Analysis (0)] |
| 16. | Wallace ZS, Deshpande V, Stone JH. Ophthalmic manifestations of IgG4-related disease: single-center experience and literature review. Semin Arthritis Rheum. 2014;43:806-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 160] [Article Influence: 13.3] [Reference Citation Analysis (0)] |